closed
Serena Vitale, National Research Council - Institute of Biochemistry and Cell Biology, Naples, Italy
Triennial Fellowship
Celiac Disease
Area: Immunology
- Grant: FC 009/2016
- Title: Dissection of T cell mediated immunity to gluten in different phases of celiac disease
- Duration: Triennial Project
- Principal Investigator: Serena Vitale, National Research Council – Institute of Biochemistry and Cell Biology, Naples, Italy
- Tutor (Head Lab): Carmen Gianfrani, National Research Council – Institute of Biochemistry and Cell Biology, Naples, Italy
Publications originated from the Project:
- Vitale S, Maglio M, Picascia S, Mottola I, Miele E, Troncone R, Auricchio R, Gianfrani C. Intestinal Cellular Biomarkers of Mucosal Lesion Progression in Pediatric Celiac Disease. Pharmaceutics. 2021 Nov 20;13(11):1971. doi: 10.3390/pharmaceutics13111971. PMID: 34834386; PMCID: PMC8623763. https://pubmed.ncbi.nlm.nih.gov/34834386/
- Vitale S, Santarlasci V, Camarca A, Picascia S, Pasquale AD, Maglio M, Maggi E, Cosmi L, Annunziato F, Troncone R, Auricchio R, Gianfrani C. The intestinal expansion of TCRγδ+ and disappearance of IL4+ T cells suggest their involvement in the evolution from potential to overt celiac disease. Eur J Immunol. 2019 Dec;49(12):2222-2234. doi: 10.1002/eji.201948098. Epub 2019 Oct 25. PMID: 31553811. https://pubmed.ncbi.nlm.nih.gov/31553811/
- Del Pozzo G, Farina F, Picascia S, Laezza M, Vitale S, Gianfrani C. HLA class II genes in precision-based care of childhood diseases: what we can learn from celiac disease. Pediatr Res. 2020 Oct 29. doi: 10.1038/s41390-020-01217-4. Epub ahead of print. PMID: 33122841. https://pubmed.ncbi.nlm.nih.gov/33122841/
Project rationale and aims
Celiac disease (CD) is associated with a broad spectrum of clinical forms and intestinal mucosal lesions. The overt-CD is characterized by atrophy of intestinal villi, presence of CD-associated HLA risk genes and serological markers, whilst potential-CD is defined by the presence of risk genes and serological markers but a histological normal mucosa. In overt-CD, CD4+ T cells reactive to gluten producing inflammatory cytokines, such as interferon(IFN)-γ and interleukin(IL)-21, have a central pathogenic role. Very little is known, instead, about the T-cell mediated response in potential-CD, and the immune mechanisms involved in the switch from normal to damaged mucosa in CD patients.
Previous studies have demonstrated that gluten-reactive inflammatory T cells are present in potential-CD intestinal mucosa, as well as regulatory T cells, these latter most likely activated as a counter regulatory mechanism to inhibit the activation and expansion of inflammatory cells. As consequence, the perturbation of the fine balance between inflammatory and regulatory T-cell pathways may be one of the factors responsible of the switching from normal mucosa to villous atrophy.
This study aimed to assess the peculiar immunological mediators involved in the progression of potential- to overt-CD mucosal lesion. In particular, this project investigated the phenotype, cytokine production and the role of gluten-reactive T cells infiltrating the small intestinal mucosa of subjects affected by these two CD conditions, in order to identify specific biomarkers of each CD phase. To address this purpose, a throughout investigation of T-cell mediated immunity to gluten was performed in gut biopsies of both children with potential-CD and overt-CD.
Research plan and results obtained
In the project, the frequency, the cell phenotype and the cytokine production of intestinal T cells were evaluated by two different experimental systems, i.e. polyclonal gluten-reactive short-term T-cell lines (st-TCLs) and ex vivo analysis on intestinal cells freshly isolated from mucosal biopsies by flow cytometry.
It was analyzed the distribution of the various T cell subsets known to predominantly infiltrate the overt-CD mucosa, such as the CD4+, CD8+ and TCRγδ+ T cells. In particular, the Figure 1 shows the cell phenotype evaluated by flow cytometry in st-TCLs. The most interesting data consisted in an expansion of TCRγδ+ T cells in the atrophic intestinal mucosa of overt-CD patients compared to their density in the morphologically normal mucosa of potential-CD children.
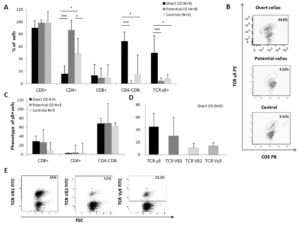
Figure 1. Increased frequency of TCRγδ+ cells in st-TCLs generated from intestinal mucosa with villous atrophy
The density of different cell subsets was analysed by flow cytometry in short-term T cell lines (st-TCLs) generated from intestinal biopsies of 5 young patients with overt-CD, 6 children with potential-CD, and 5 non-CD controls. The cell phenotype was evaluated in st-TCLs after 21-24 days from the culture set-up. (A) Overall percentage of cell subsets and (B) representative flow cytometry dot plots of CD3+TCRγδ+ cells from each group of subjects are shown. (C) The phenotype of TCRγδ+ cells is shown. Data indicate median values ± SD of all experiments. (D) Mean frequency of TCRγδ+ T cells that express Vδ1, Vδ2 and Vγ9 chains of TCR γδ from st-TCLs of 3 overt-CD patients and (E) representative flow cytometry dot plots of Vδ1, Vδ2 and Vγ9 positive cells from one subject. The Student t-test was applied to evaluate statistical significant differences among the groups. A p value < 0.05 was considered statistical significant and labelled with asterisk *p <0.05, ** p <0.01, *** p <0.001.
The expanded TCRγδ+ T-cell population (Fig. 1A and B) was composed mainly of CD4CD8 double negative cells (Fig. 1C) expressing the Vδ1 chain (Fig. 1D and E). When we investigated the profile of cytokine production of intestinal T cells, remarkably we observed a substantial reduction of IL4+ T cells in the damaged mucosa compared to potential-CD mucosa. As shown in Figure 2, the great majority of cells releasing IL4 found expanded in potential-CD mucosa were CD4+ T cells (Fig. 2A and B), and approximately half of them produced also IFN-γ (Fig. 2C).
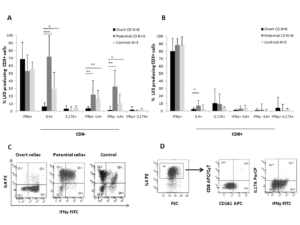
Figure 2. The villous atrophy of the small intestinal mucosa is associated with low frequency of IL4 producing CD3+ cells
IL17A-, IFNγ-, IL4-producing cells were detected in st-TCLs by intracytoplasmic staining after 6 hours of mitogen (PMA/Ion) stimulation. The frequency of cytokine producing CD3+ cells, both CD8- and CD8+ cells, were analysed in 6 overt-CD patients, 6 potential-CD patients and 5 controls. (A) Percentages of cytokine producing CD8- cells and (B) percentages of cytokine producing CD8+ cells in the gate of CD3+ cells are shown. (C) Representative dot plots of CD3 positive CD8 negative cells that producing IL4/IFNγ from each group of subjects are shown. (D) Dot plots of IL4+ T cells are reported from a representative potential-CD subject. Data indicate median values ± SD of all experiments. The Student t-test was applied and a p value < 0.05 was considered statistical significant, *p <0.05, ** p <0.01, *** p <0.001.
Moreover, IL4+ T cells were mostly classical Th2 cells, as negative for CD161, and did not produce IL17A (Fig. 3D). These results were confirmed by ex vivo analysis (data not shown). Furthermore, the percentage of IL4+ T cells inversely correlated with TCRγδ+ T cells, thus suggesting that the combined detection of these two cell subsets represent a useful approach to characterize the CD main forms.
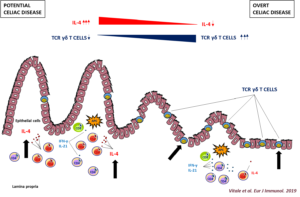
Figure 3. The transition from normal to damaged intestinal mucosa in celiac disease
The intestinal mucosa of potential-CD condition displays an increase of IL4-producing T cells whilst TCRγδ+ cells are increased in overt-CD. The transition to villous atrophy in CD patients is characterized by an expansion of TCRγδ+ T cells and by a concomitant disappearance of IL4+ T cells in the gut mucosa.
Experimental design and methodologies
St-TCLs were raised from intestinal cells after enzymatic digestion of mucosal biopsies, by stimulation with irradiated autologous peripheral blood mononuclear cells, deamidated peptic-tryptic digest of gliadin, and with IL-2 and IL-15 as grow factors. In both in vitro and ex vivo systems, the frequency, the cell phenotype (CD3, CD4, CD8, TCR γδ, TCR αβ, CD161, Vδ1, Vδ2, and Vγ9) and cytokine production (IL-4, IL-17A, and IFN-γ) were investigated by multiparametric flow cytometric analyses. Cytokine positive cells were evaluated after PMA/Ionomycin stimulation. The correlations between variables were assessed by the Spearman and/or Pearson correlation coefficient.
Potential pitfalls and caveats
The recovery of intestinal cells than can be obtained from each mucosal biopsy is, in general, very limited, and it has not always been possible to perform all the planned experiments. To overcome this limitation, and to obtain consistent results, the number of patients from whom intestinal samples were obtained was increased compared to that initially programmed in the research proposal (total number of subjects enrolled for the study: 12 age-matched non-CD controls, 18 potential-CD and 29 overt-CD).
Although the IL4+ and TCRγδ+ T cell data are very promising, further investigations are needed to make these biomarkers useful as a diagnostic tool in CD.
Conclusions and discussion
The main results obtained during the 3 years of project demonstrated that intestinal TCRγδ+ and IL4+ T cells are promising immune-specific biomarkers that discriminate between overt- and potential-CD condition. The transition from histologically normal (potential-CD) to atrophic intestinal mucosa (overt-CD) is characterized by an increased epithelial infiltration of IFN-g producing TCRγδ+ T cells, that express Vδ1 chain, and a lamina propria expansion of Th1 cells releasing IFN-g and an almost disappearance of IL4 producing Th2 cells. These latter cells were found at higher frequency in the normal mucosa of potential-CD patients, thus suggesting a regulatory role on IFN-g producing Th1 cells.
The combined detection could represent a useful approach to characterize the different CD forms, given the indirect correlation between the percentages of TCR γδ+ and IL4+ intestinal T cells in CD patients.
The assessment of these T cell populations frequencies could be important to predict the possible switch from potential-CD to overt-CD condition, as illustrated in Figure 3. Interestingly, the data suggest that these two biomarkers could be useful to predict the development of damage already from the early changes, as demonstrated by the higher density of TCR γδ+ T cells and concomitant low frequency of IL4+ T cells in potential-CD young patients.
Collectively, the results obtained during the 3-years FC project strongly suggested that IL4+ and TCRγδ+ T cells could be new CD immune-specific biomarkers valuable to characterize the different CD forms, and could provide diagnostic tools to predict the disease progression.
